Basic to Clinical
Co-treatment helps target nerve fibres associated with neuropathic pain.
Inhibition of mechanical allodynia in neuropathic pain by TLR5-mediated A-fiber blockade.
Mechanical allodynia, when normally innocuous touch is perceived to be extremely painful, is associated with various types of neuropathic pain. There are several types of nerve fibers involved in mechanical allodynia, but recently there has been a growing awareness of the involvement of Aβ nerve fibers—myelinated fibers known for their medium to large diameter. Until now there have been very few tools to target these specific Aβ fibers therapeutically, as there have been for other kinds of nerve fibers. In this study, researchers identify a molecule known as Toll-like Receptor 5 (TLR5) that seems to be specifically associated with these group Aβ fibers. In order to target a drug to these group Aβ fibers, the scientists essentially had to “unlock” the receptor using its “key,” a molecule called flagellin, and co-treat with a drug called QX-314, which is a derivative of the well-known anesthetic lidocaine. When the researchers added flagellin and QX-314 to large diameter A fibers in a dish, they blocked sodium currents, thereby functionally blocking the nerve activity. They also tested the effects of this co-treatment in animal models of neuropathic pain, including neuropathy associated with chemotherapy, diabetes, or nerve injury. Across these models, mice treated with the experimental therapy exhibited less response to a mechanical stimulus, a way of testing for mechanical allodynia. Further, the scientists showed that the neuropathy symptoms in transgenic mice that lacked TLR5 were not reduced after the co-treatment, suggesting that this is a very specific way of targeting the group Aβ fibers. The results from this study enable better characterization of these important nerves and could lead to better treatment for many kinds of neuropathic pain.
Computed Tomography Imaging Helps Target Pain-Transmitting Nerve Cells
The burning from chili peppers is a familiar sensation to many people. Capsaicin, the chemical in chili peppers that cause that burning sensation, activates a receptor called TRPV1. TRPV1 is primarily expressed in nerve cells whose job it is to transmit pain signals stemming from noxious heat or inflammation. It is largely absent in other nerve cells responsible for sensory or motor function. Because of its specificity to these nociceptive neurons, TRPV1 could be a good therapeutic target for inhibition of pain without disrupting other important functions of surrounding nerves. In this study, researchers injected a naturally occurring chemical called resiniferatoxin (RTX), a potent activator of the TRPV1 receptor, into the nerve cells of pigs with the help of computed tomography (CT)-guided scans. RTX is so potent that at high doses it quickly compromises the TRPV1-neurons and causes them to die. Using the CT scanning as guidance, the researchers injected RTX into nerves on one side of the spine and a control “vehicle” on the other side of the spine. After the pigs recovered, the researchers tested their response to a brief laser heat stimulus in the skin area where the nerves connected to the injected portion of the spine. They found that the pigs were much slower to respond to the stimulus when tested on the side which corresponded to the RTX-treated nerves. This finding suggests that the ablation of those nerve cells by RTX reduced pain transmission. Further, the researchers found that the injected tissue areas had reduced amounts of TRPV1 transcript, and significantly fewer TRPV1-neurons, suggesting that the RTX treatment reduced the overall number of these pain-sensing neurons. In order for this treatment to be clinically useful one day, it is important that it not disrupt motor function. The researchers assessed and found no sign of gait impairment or disability in any of the animals, indicating the CT scan guidance resulted in very specific injection areas. This study shows that with the right tools, RTX might one day be used as a potent block for peripheral painful conditions. In the near future, this would be especially useful in many different neuropathies as well as visceral pain stemming from the pancreas or kidney. With continued progress, it is possible that the utility of RTX could broaden into a wider array of pain conditions, such as phantom limb pain, metastatic cancer pain, and osteoarthritis.
Pain Mechanisms
Mindfulness Meditation Activates Different Brain Regions than Placebo
There have been several studies indicating that mindfulness meditation can help alleviate different kinds of pain. Mindfulness meditation is a practice of thinking non-judgmentally about surrounding sensory events, often with a focus on breathing. While studies have shown that this kind of meditation can reduce pain, it has been unclear whether this is distinct from the neural mechanisms that can make placebo treatment effective. Using healthy volunteers who received a brief heat stimulus, researchers compared the effects of true mindfulness meditation, “sham” mindfulness meditation (which involved sitting quietly without specific mindfulness instructions), treatment with a placebo cream, and simply reading a book, on pain intensity and unpleasantness ratings. All four conditions reduced pain intensity and unpleasantness compared to the levels the same volunteers experienced prior to the interventions, however mindfulness meditation had a more significant effect than any of the other treatments. Researchers not only had the volunteers rate the intensity and unpleasantness of the pain, but also performed functional magnetic resonance imaging on the volunteers’ brains. Compared to the sham meditation group, researchers found less activity in brain regions associated with generating the perception of pain, specifically the regions of the thalamus and periaqueductal gray matter, in the group that had performed mindfulness meditation. Additionally, they found that there was more brain activity in regions such as the insula and secondary somatosensory cortex, which is related to sensory processing, and the orbitofrontal cortex, which is associated with reevaluating and attempting to regulate one’s emotions. Importantly, these novel findings suggest that mindfulness meditation may induce pain-reducing brain activity distinct from that produced by placebo. In the future, these methods could be further tested in individuals suffering from chronic pain as well.
Risk Factors & Causes
Psychosocial Factors Predict Post-Operative Pain and Quality of Life Outcomes in Children

Pain can be influenced not just by physical factors, but also psychological and social ones. Studies have established that these “psychosocial” factors are predictive of post-operative pain in adults undergoing surgery. How these factors affect children has not been well established, however. With around 5 million children undergoing surgery annually in the United States, this question of risk factors could guide prevention or intervention strategies to limit post-surgery pain. In this study, researchers assessed a number of behavioral and psychosocial factors in children, and their caregivers, both before and after major surgery to identify predictors of better or worse pain and quality of life outcomes. These measurements included a baseline assessment of pain, a health-related quality of life measurement, sleep assessment, and measurements of anxiety and pain catastrophizing. Pain catastrophizing is the act of negatively exaggerating a painful experience, and this effect was measured from both the child and parent perspective in the week leading up to surgery and 2 weeks afterwards. The authors found that shorter pre-surgery sleep duration and greater parental pain catastrophizing (but not catastrophizing from the children themselves) were associated with greater post-surgery pain intensity. From a broader perspective, the authors also measured health-related quality of life, which considers physical, emotional, social, and school function. Greater child anxiety measurements pre-surgery predicted poorer health-related quality of life after surgery. Taken together, these results suggest that there are pre-surgery modifiable factors that could potentially be influenced to positively affect the pain and quality of life outcomes of children after surgery.
Surveillance & Human Traits
Estimating Pain Prevalence and Severity in US Adults
Estimates of pain prevalence and severity in adults: United States, 2012.
Measuring pain is challenging due to its subjective nature. Current healthcare standards to measure pain rely on self-report using a simplistic 10-point scale that doesn’t take into account the experience or severity of pain for an individual. A better understanding of the prevalence of pain and pain characteristics is needed to improve pain management and treatment. Furthermore, a better understanding of pain in diverse populations (racial/ethnic, gender, age) is needed. The National Health Interview Survey asks questions related to daily pain, pain persistence and the extent to which the pain is bothersome in frequency and intensity. The following study analyzed data from the 2012 survey to estimate pain prevalence and severity in adults. Approximately 126 million (55%) survey participants reported some pain in the last 3 months. When looking at specific populations, the results showed that females, older individuals, and non-hispanics were more likely to report pain whereas non-hispanic asians were less likely. Of those who reported some pain, 25 million reported daily chronic pain. The study used Washington group pain categories which categorizes pain severity based on the persistence and bothersomeness of pain. There are 4 categories ranging from low severity (cat. 1) to high severity (cat. 4). Those reporting the most severe pain were more likely to have a higher number of painful comorbid health conditions (eg., fibromyalgia, migraine, back pain) than those reporting less severe pain. More severe pain increased the probability of being in an overall poorer health state. The study further examined the relationship between pain severity and demographic characteristics including race, ethnicity, language preference, gender and age. Non-hispanic asians, preferring english and Hispanic whites, not preferring English were more likely to be pain free and less likely to have category 3 pain than non-hispanic whites, non-hispanic blacks and Hispanic whites, all preferring English. Female non-hispanic whites and blacks, preferring English were more likely to have higher rates of category 3 or 4 pain severity than their male counterparts. Lower prevalence of category 3 or 4 pain severity was found in the 18-44 age group compared to older age groups. These data shed light on the extent of pain suffering and begins to identify subpopulations for which certain interventions may be more beneficial.
Tools/Instruments
Advancing Optogenetics With Miniature Devices
Wirelessly powered, fully internal optogenetics for brain, spinal and peripheral circuits in mice.
Soft, stretchable, fully implantable miniaturized optoelectronic systems for wireless optogenetics.

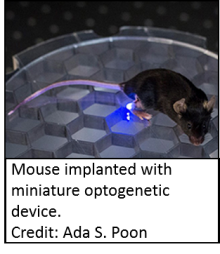
Optogenetics, a technique in which light-sensitive proteins are expressed in specific cell types allowing for the activation of these cells when exposed to specific wavelengths of light, allows for specific spacial an temporal control when activating neurons. This has revolutionized the study of neural circuits in awake, behaving animals. However, some aspects of the technology limit the utility of optogenetics when studying animals in a normal environment. Traditional optogenetics setups involve a box that produces light with a fibre-optic cable implanted into a mouse where it can reach the cells to be activated. The limitations of this system are numerous. The cable acts as a tether for an animal, restricting its movement making behavioral data difficult to collect accurately. In addition, optogenitically available cells were limited to the brain, because the cable requires a large, stationary bone mass, such as the skull as an anchor. Some advances have been made allowing for wireless control of lights, but these have still had external components that could be damaged by the animal being studied or it’s cage-mates. Here we highlight two groups that have developed small, implantable optogenetic systems to address some of these problems.
Park et al developed a miniature, flexible system that can be implanted over a variety of neural interfaces, such as the spinal cord or peripheral nerves. This system is powered by radio frequencies that are recognized by a flexible antenna. With no external components, this system can be implanted into a mouse and wirelessly activated while the mouse is performing normal activities and even while it is in its home cage. This group implanted the device over the sciatic nerve or spinal cord of mice in which sensory neuron cells could be activated with blue light. With the devices implanted, but not activated, the animals behaved normally. When the appropriate radio frequency was present, the animals showed behaviors consistent with pain caused by activation of sensory neurons in the sciatic nerve or spinal cord.
Montgomery et al developed miniature implants with highly efficient LEDs powered by radio frequencies emitted from a grid that the mouse can walk on. This implant can be built in the lab with readily available materials and can be implanted under the skin to activate sensory neurons in the periphery. This group implanted these devices in mouse hindpaws. Again, when the implants were not activated, the animals behaved normally and when the light was turned on, they exhibited behavior consistent with a pain in the paw.
These studies show that miniature wireless implants can activate neurons that were not accessible with traditional optogenetic techniques. They will allow for new types of studies and a wider range of cell types being tested.
